AI Enhances Accuracy in Prostate Cancer Detection: A Multinational Study
In a world where artificial intelligence is rapidly transforming healthcare, a recent multinational study demonstrates how AI could significantly boost the detection of clinically significant prostate cancer (csPCa) in patients undergoing biparametric MRI (bpMRI) prostate exams. Conducted across 53 facilities in 17 countries, this study casts a spotlight on the promising intersection of technology and medicine.
Key Findings: A Boost in Sensitivity and Specificity
Published in JAMA Network Open, the research assessed AI software developed by the Prostate Imaging-Cancer AI (PI-CAI) Consortium and its effectiveness in interpreting MRI scans of 360 men classified with PI-RADS scores of 3 or higher—indicating a likelihood of prostate cancer. Out of this cohort, 122 men were diagnosed with csPCa.
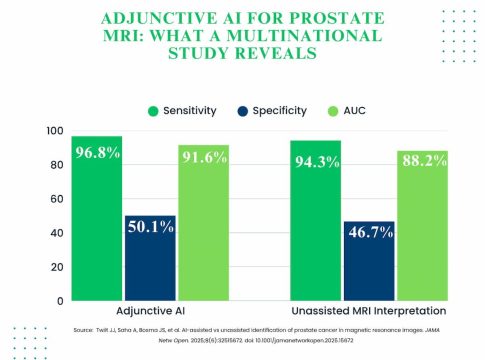
Notably, the incorporation of AI led to improvements in diagnostic performance:
- Sensitivity increased by 2.5% (96.8% with AI vs. 94.3% without).
- Specificity improved by 3.4% (50.1% with AI vs. 46.7% without).
Moreover, the area under the receiver operating characteristic curve (AUC)—a key performance metric—rose from 88.2% to 91.6%, showcasing AI’s ability to reduce false positives by ten cases when compared to traditional methods.
AI’s Influence on Radiologist Performance
One of the study’s intriguing findings revealed that non-expert radiologists benefited more from AI assistance than their expert counterparts. Non-experts saw a 3.7% boost in sensitivity and a 4.3% increase in specificity, while experts experienced more modest gains of 1.5% and 2.8%, respectively.
This trend suggests that AI could help bridge the performance gap between varying levels of radiological expertise. Non-expert radiologists using AI actually achieved higher AUC scores than experts operating without AI support, underlining the technology’s potential to democratize healthcare diagnostics.
Implications for Clinical Practice
The findings hold significant implications for clinical decision-making. With AI adjusting PI-RADS scores in 33% of assessments—including a notable 17% reclassification from positive to negative—radiologists may reconsider biopsy decisions, potentially reducing unnecessary procedures and improving patient care.
However, it’s essential to acknowledge the study’s limitations. Conducted retrospectively and largely on a single MRI system, it raises questions about the broader applicability of the AI software. Also, the controlled online reading environment may not fully mimic real-world settings, making the transition from research to routine clinical use an important next step.
A Promising Future for AI in Healthcare
As AI technologies continue to evolve, their integration into healthcare is not merely an enhancement but a necessity for improving outcomes. This study reaffirms the potential of AI in not just augmenting diagnostic accuracy, but also in leveling the playing field for medical professionals at different stages of their careers.
As we look ahead, the challenge will be ensuring these tools are effectively implemented in clinical practices worldwide, ultimately driving better patient outcomes in prostate cancer detection and beyond. The implications of such advancements might well reshape the landscape of medical diagnostics, paving the way for a more efficient and equitable healthcare system.

Writes about personal finance, side hustles, gadgets, and tech innovation.
Bio: Priya specializes in making complex financial and tech topics easy to digest, with experience in fintech and consumer reviews.